Every paramedic gets the same types of medical scenarios in their certifying course or refresher class. There’s the grassy field where a bee will have been involved, causing an anaphylactic reaction. Another one will involve an elderly person at home in the summer with closed windows where your detective skills will surmise that a heat stroke has most likely led to his change in consciousness. And if there’s heart attack scenario it will usually involve someone shoveling snow.
Shoveling snow is considered to be such a cardiac risk specific mention of it is made in many cardiac journals and as a warning to patients who have had myocardial infarction (MI), or heart attacks, in the past or are at risk for it. The combination of sudden strenuous labor and the cold air that is already constricting your blood vessels make it especially dangerous for someone who is already compromised.
When you’re being tested on these scenarios, either acting them out with mannequins or describing what you’d do to an instructor one on one, there are rarely curve balls thrown in to confuse you. The instructors aren’t interested in your clever abilities in finding a hidden medication bottle or poking holes through the family’s story about how the event happened. They just want to know that you can remember the protocol and apply it properly.
Rarely in real life are scenarios this cut and dry. Real patients lie to get out of going to the hospital or exaggerate to get seen faster. Sometimes medication bottles, or a drug habit, are well hidden and require real sleuthing skills. Or sometimes the patients list of symptoms is so long it’s difficult to figure out what the real problem is. But once in a while everything is exactly the way it is in the textbooks, probably the reason why they’re used as examples.
It was a snowy, winter day that my partner and I had made our way to the far off corners of Brooklyn thanks to limited unit availability and the far away hospital requests of several patients. We enjoyed leaving the confines of our assigned area which gave us opportunities to eat better and deal with completely different hospital staffs. We now found ourselves assigned to a predominantly Russian-speaking area of the borough where my partner had worked as an EMT. He knew the streets well so we didn’t have to spend large amounts of time flipping pages in our paper map book trying to find the address.
When we got to the apartment our patient, a large dark haired man with a Russian accent, was exhibiting the classic ‘Levine sign’. It’s a sometimes subconscious act of holding a fist on the chest near the heart. If this were part of a training scenario it would be the first thing that would alert the paramedic to think ‘heart attack’ or ‘myocardial infarction’ (MI). The man seemed a bit preoccupied, one could describe it as anxious (#2 for sign and symptoms), and he said he had no patience for us. He was a busy man and would not be going to any hospital. His wife had been foolish to call.
The wife appeared annoyed but was also clearly worried. “Just let them check you. Please. If it’s nothing they can go,” she said. The man grew more irritated but he decided to appease the wife and get checked out, possibly just so he could show her what a waste of time this all was. He rolled up his sleeve and demanded that we take his blood pressure so his wife would see how healthy he was.
His skin was pale (#3), cool (#4), and very sweaty (#5). When I took his blood pressure it was high, very high (#6). Impatiently, he demanded that we should take it again, we must have gotten it wrong. But it was still high the second time. He rolled up his other sleeve. He now told us that his left arm was numb (#7) so the pressure couldn’t be accurate in that arm. A try with the right arm was really no different. The wife gave a smug nod that infuriated the patient.
He insisted that he was a strong person, physically and mentally. As the building manager, he had a very active schedule and many things were left to be done. He couldn’t rely on anyone else. The people of the building had become accustomed to things being fixed correctly and they knew he was the only man for the job. That morning, when other building managers would have slept in, waiting for the impending snow to actually fall, our man was out there salting the roadways ahead of time. Once we heard that he had done all the shoveling (#8), with an actual shovel and not even a snowblower, when the snow had finally came, we didn’t even need an EKG. This guy was having an MI.
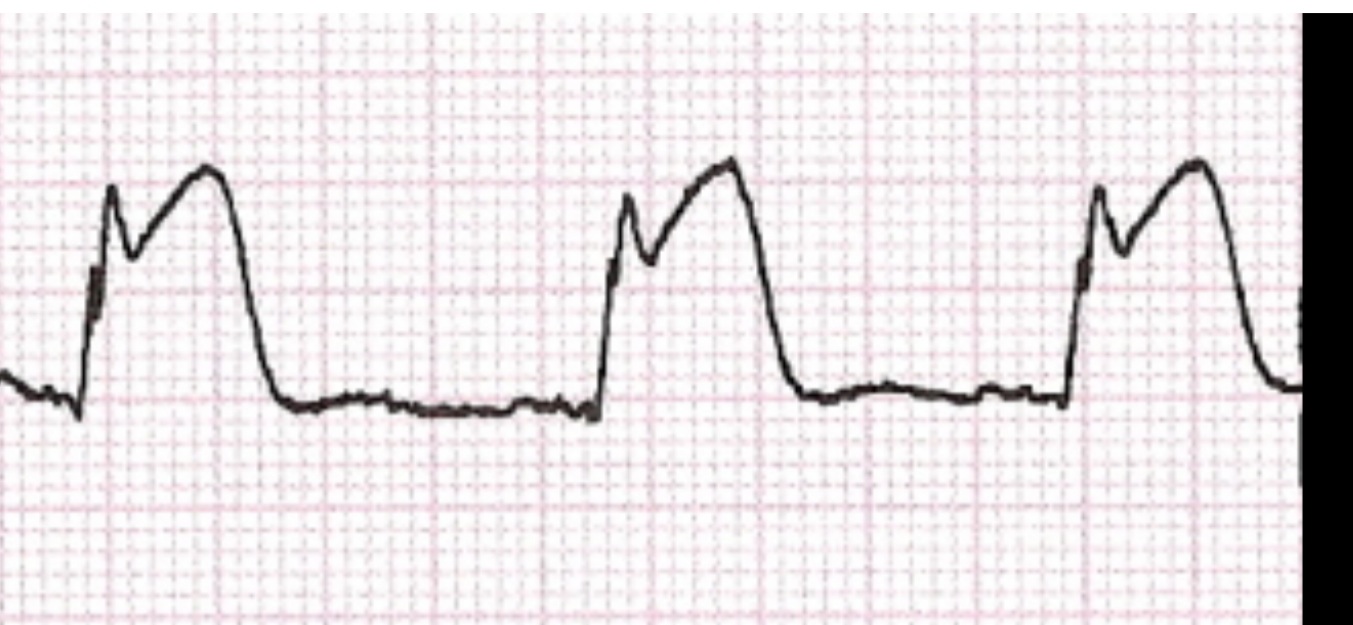
But we put our patient on the monitor anyway, of course, and it showed a rapidly evolving, life threatening MI. When we presumptively diagnose a heart attack we are usually only looking for tiny incremental changes in the EKG. It’s often only a small, two millimeter height difference on the graph paper. But his were so high they didn’t even need to measured. We could see them from across the room. The shapes of his complexes are even called “tombstones”.
None of this convinced the patient however. He was fine, he told us. He wasn’t one of these “sissy-boys” who needed to see a doctor for every ache and pain. He would lay down for a few minutes and then, when his chest pain subsided, he would get back to work. More snow was coming. He had heard it on the news.
We told him in every way possible that he was having a heart attack and it was progressing. One or more of the vessels supplying his heart was clogged, which was depriving more and more areas of his heart of oxygen. With current treatments available this problem could very potentially be reversed if we got him to a STEMI center quickly. They would quickly put in a stent and blood flow could be restored. His heart would most likely function the way it had before. But he had already waited some time and it looked as if it was going to take even longer to convince him.
We explained about cardiac death and the whole ‘time equals muscle’ philosophy, meaning that the longer the heart goes without oxygen the more muscle mass that dies. He would not hear any of it. His chest hurt because he was sore from shoveling snow. We were stupid to not see that. Didn’t we know how strenuous it is to shovel snow? He had shoveled around the whole building, down pathways and parts of the parking lot. Of course he was sore, he had exerted himself the way he always does, giving 110% to his residents. Couldn’t we see how strong he was to be able to accomplish all he did today? We had probably never shoveled snow or we would have understood the muscle soreness.
He thought that we had taken his wife’s side in this argument. He would need to placate us, he felt, in order to get rid of us. So when he was offered a spray of nitroglycerine under his tongue he accepted. He also took the aspirin we gave him. We continued to watch his EKG and continued to take vital signs.
Shortly after the nitroglycerine his face lit up. “The pain. It’s gone. All gone,” he told us happily. “See? You cured me. Now you can leave.” It was hard to know if the pain was actually gone but saying that our spray had worked bolstered our argument that his pain was cardiac. Nitroglycerine wouldn’t have worked for regular muscle soreness. The building manager was frustrated that he had been tricked.
We spent a considerable amount of time trying to break through his wall of defensiveness. The internet existed back then and the couple had a computer so we had the man look up his signs and symptoms. We asked him to look up the EKGs of people having heart attacks and compare them to his. The best example we were able to Google had much smaller tombstone complexes. “Look,” he told us. “Mine are better!” The larger complexes, he explained, were due to his superior physical conditioning. The person with the EKG on the internet probably wouldn’t be able to shovel miles of snow the way he had.
Everything short of shadow puppets had been used to try and convince our patient to seek help at the hospital for an ongoing event that could very likely kill him. We tried to understand his fear of the hospital which he denied was the reason. We even offered to take him to a different hospital, one of his choice, but he was not interested. And he had every right to refuse. If he didn’t consent to go we couldn’t force him. The patient knew that we couldn’t force him.
“This is America. Not Communist Russia. No one can just come and force me to gulag. You understand gulag, correct?”
Yes we understood. But because he had an evolving, life-threatening event going on he would be required to speak to our doctor on our taped line and tell him that he was refusing. Perhaps even, our MD could convince him to go. We called up our telemetry number and told the physician what was going on. He initially thought we were doing a routine STEMI presentation so that he could notify the hospital. By going through this procedure the patient pretty much goes directly upstairs to the catherization lab, saving time and muscle. “OK, I’ll contact them immediately. What’s your ETA?” he asked.
“He doesn’t want to go,” we told him.
“Doesn’t want to go? That’s crazy. He will die.”
“Yup.”
We put the patient on the phone and heard him get defensive less than a minute into the call. We could hear the doctor patiently explain the entire thing, going into great detail about the heart and how it was being damaged and what would happen if he didn’t go. But none of it mattered. He wasn’t going. No one could make him. He was not having a heart attack. OK you think it’s a heart attack, big deal. I don’t care if it is, he told him. He was fine. He understood the risks. He told the doctor about the gulags of communist Russia. If anything changes he understood he could call back. He handed the phone back to us.
“Well, we did our best. Take the RMA (refusal of medical assistance)”
The patient breathed a big sigh of relief. Finally we were leaving. His personality did a complete turnabout now that the pressure was off. He was gracious and friendly as he signed our paper. He hoped we hadn’t been greatly inconvenienced. He was happy we could finally go out and help all the people who really needed us.
It’s so surreal to look at someone who is dying and know what is happening. You try to look for something different, maybe an aura. Or you try to feel something, to perhaps boost your intuitive powers so that the next time you get someone like this, but without the telltale signs, you’d know, you’d recognize that feeling. But there was nothing, no aura, no unusual sensation. On the outside, he was just a regular guy with elevated vitals who was turning a little gray. It makes you feel more helpless than ever. You can’t even learn from the experience. The one big thing that helps EMTs and paramedics to cross over a psychological hurdle, when you’ve got someone critical, is the knowledge that you can actively do something to help. Even if it doesn’t work in the end, you tried and you can console yourself with that. Knowing that you have it in your power to help stop the cascade of medical disasters occurring in that person but are unable to provide it makes you feel useless and small.
We asked again before leaving to please reconsider. His wife was crying and begging him to go. But he just happily opened the door and bid us good-bye.
After the call we went to the nearby station my partner had done his EMT years at. He said hello to some people he knew and used to work with and introduced me. Our radios were tuned to a different frequency because we belonged to a different section of the city, so we normally would not have heard the call go out for a cardiac arrest at the address we had just left from. But because we were talking to people who did work in that section we heard it come over on their radios. We just looked at each other sadly and shook our heads. It had been less than an hour. Shortly after that we heard the crews that responded give a signal indicating that resuscitative efforts had failed and that the patient had been pronounced on scene.
“You guys RMA’d that guy?” someone asked. “I guess you guys are in trouble now.” They looked at us as if we had happily taken his signature as soon as we walked in.
“No,” explained my partner to the young EMTs. “We tried. But this isn’t communist Russia where we can just haul you off to the gulag.”
Recent Comments